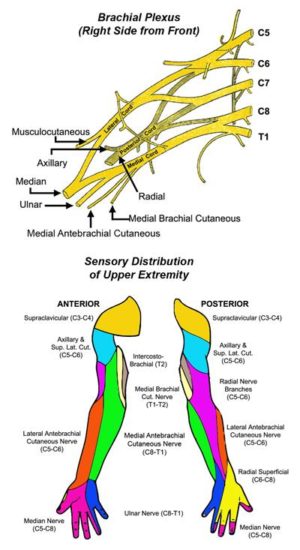
The principal nerves serving the upper extremity arise from the spinal nerve roots at levels C5, C6, C7, C8, and T1. Within a few centimeters of leaving the spine, these five individual nerve roots bundle together and interconnect with each other to form the brachial plexus. The nerves of the brachial plexus pass directly through the scalene triangle before passing underneath the clavicle to the upper arm, where they begin to branch into individual peripheral nerves. These nerves and their branches serve all of the motor and sensory functions of the arm and hand.
The phrenic nerve is an additional nerve in the area of the thoracic outlet. It arises as a small branch at the top of the scalene triangle and passes vertically and across the front of the anterior scalene muscle. The phrenic nerve then passes behind the subclavian vein and deeper into the chest, where it runs down past the heart and lung to innervate the diaphragm. Contraction of the diaphragm occurs particularly during deep breathing and respiratory exertion.
Another nerve in the area of the thoracic outlet is the long thoracic nerve. The long thoracic nerve forms from three smaller nerves within the middle scalene muscle and passes over the midportion of the first rib. It then passes back underneath the scapula, where it innervates the serratus anterior muscle. The serratus anterior functions to help keep the scapula close to the chest wall during arm elevation and rotation.